I’ve written frequently about Gov. Roy Cooper and DHHS Sec. Mandy Cohen’s misleading use of data on COVID-19 in North Carolina, a disreputable and insulting practice with which our news media choose to be complicit.
They have especially made use of reported new cases of the virus to keep the public alarmed that the virus is getting worse and that Cooper’s increasingly stringent mitigation measures are ever needed. Politically, it’s working. That doesn’t make it right.
As I’ve shown, the amount of new cases of the virus is tightly linked to the amount of new testing, since the percent positive has been remarkably steady since late April/early May. Only if you’re in possession of a memory will you recall that in the early months of the disease, the state health establishment actively discouraged people from getting tested for COVID-19 unless they were very sick.
In the words of not one, not two, but six former state health directors — namely, Robin Gary Cummings, MD; Leah Devlin, DDS, MPH; Jeff Engel, MD; Laura Gerald, MD, MPH; Ron Levine, MD, MPH; and Hugh Tilson, MD, DrPH — from March 23:
Don’t seek testing for COVID-19 if you have a mild illness.
We know this recommendation may come as a surprise. However, the vast majority of people who get COVID-19 will have mild illness and recover at home. When people leave their home for testing, they could expose themselves to COVID-19 if they do not already have the infection. If they are infected, they can expose someone in the community, including people who are at high risk, or a health care worker. We need to reduce the chances for further spread and protect our health care system, so it is there when people need it most.
If you’re not sick enough to need medical care, a positive COVID-19 test will not change what you or your doctor do. Anyone who has fever and signs of respiratory illness including cough should stay home until at least 7 days after the first day of illness AND until they have been without fever for three days and other symptoms are improving. People who have been in close contact with an ill person are urged to stay home as much as possible and monitor themselves for signs of illness. During this phase of the outbreak, testing is most important for severely ill patients, health care workers, and persons in nursing homes and other vulnerable populations.
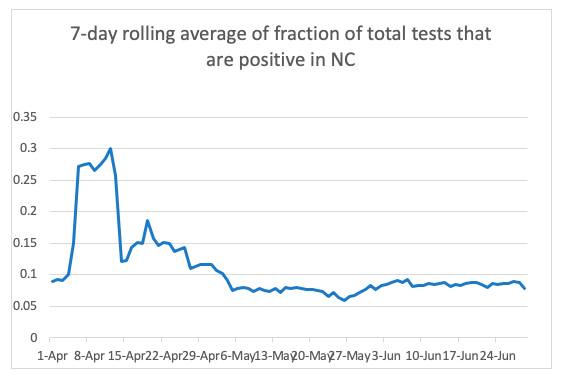
In the early months, testing was reserved for the very sick. Those tests would yield higher percent positives, but there were fewer of them. Once testing increased and expanded beyond the already very sick, the percentage of tests resulting in positive cases fell dramatically and has stabilized (for discussion, see Dr. Donald R. van der Vaart’s piece on The Fog of COVID-19 Data: North Carolina is “holding at a steady pace”):
Meanwhile, testing has continued to increase:
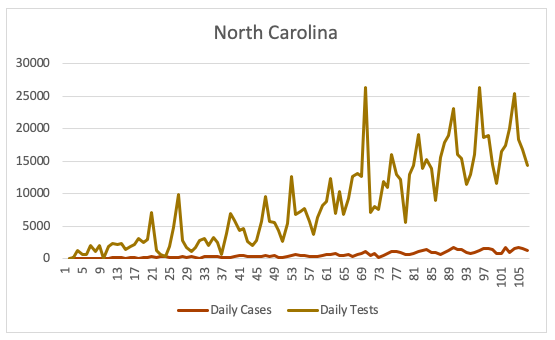
In short, we’re testing more, we’re finding more cases, and we’re finding more asymptomatic and barely symptomatic (“not sick enough for medical care”) cases, so therefore we’re witnessing a falling proportion of cases that are deadly.
(There are other factors at play as well: earlier cases likely involved more vulnerable populations, viruses tend to weaken over time, newer cases are increasingly among age cohorts that are significantly less likely to succumb to the virus, etc.)
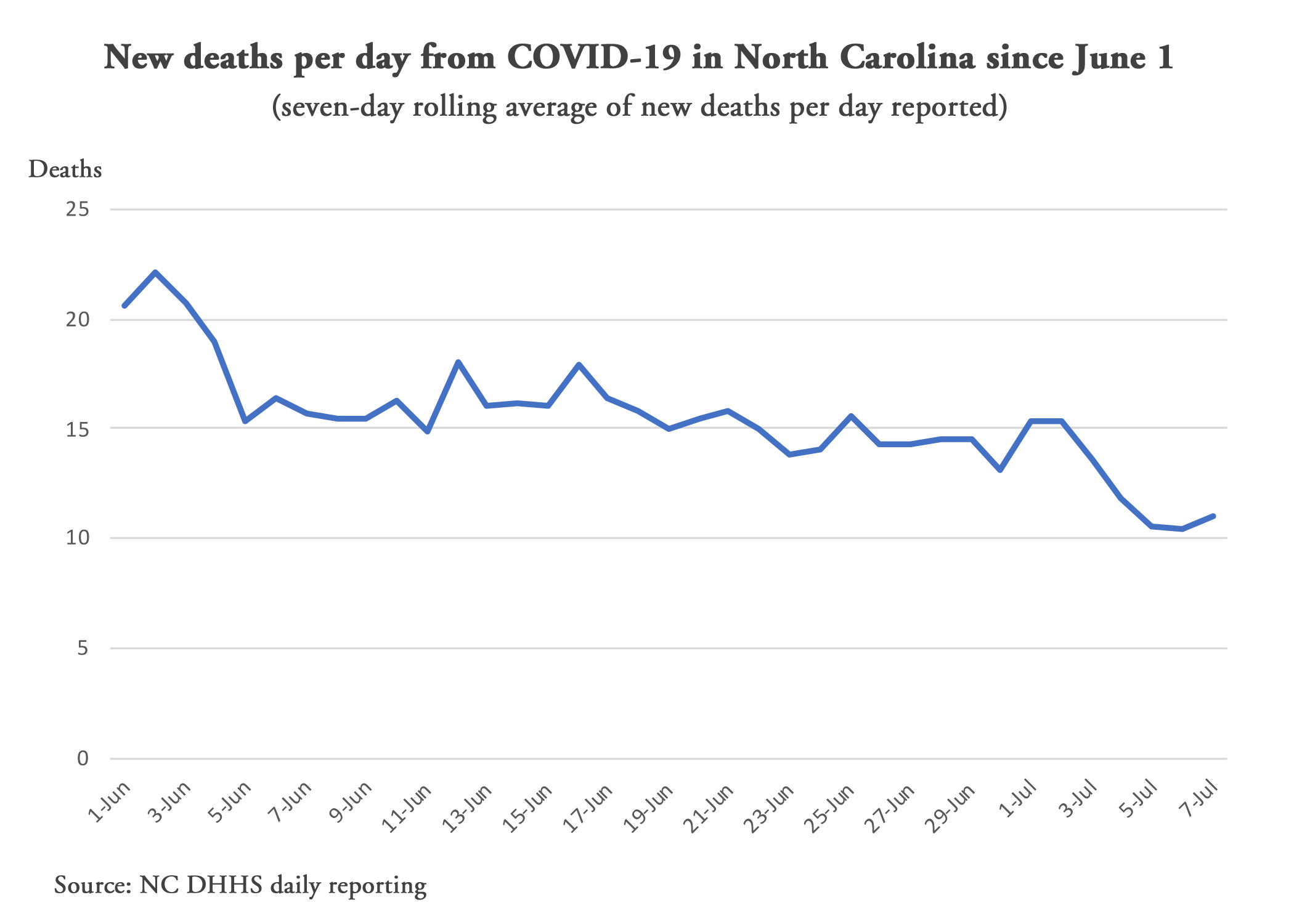
The graph atop this post shows exactly that. The seven-day rolling average of deaths per day have been steadily falling all month. (Using a seven-day rolling average helps smooth out the data to examine a trend, so that a one-day reporting spike or valley doesn’t give a false impression of the overall trend of the data.)
As you can see from the graph above, as of today, the average deaths per day is half of where it was on June 2.
Here’s another way of looking at it. This is a rough way of looking at how deadly the known cases are. It takes the seven-day rolling average of deaths and compares it to the seven-day rolling average of cases three weeks prior.
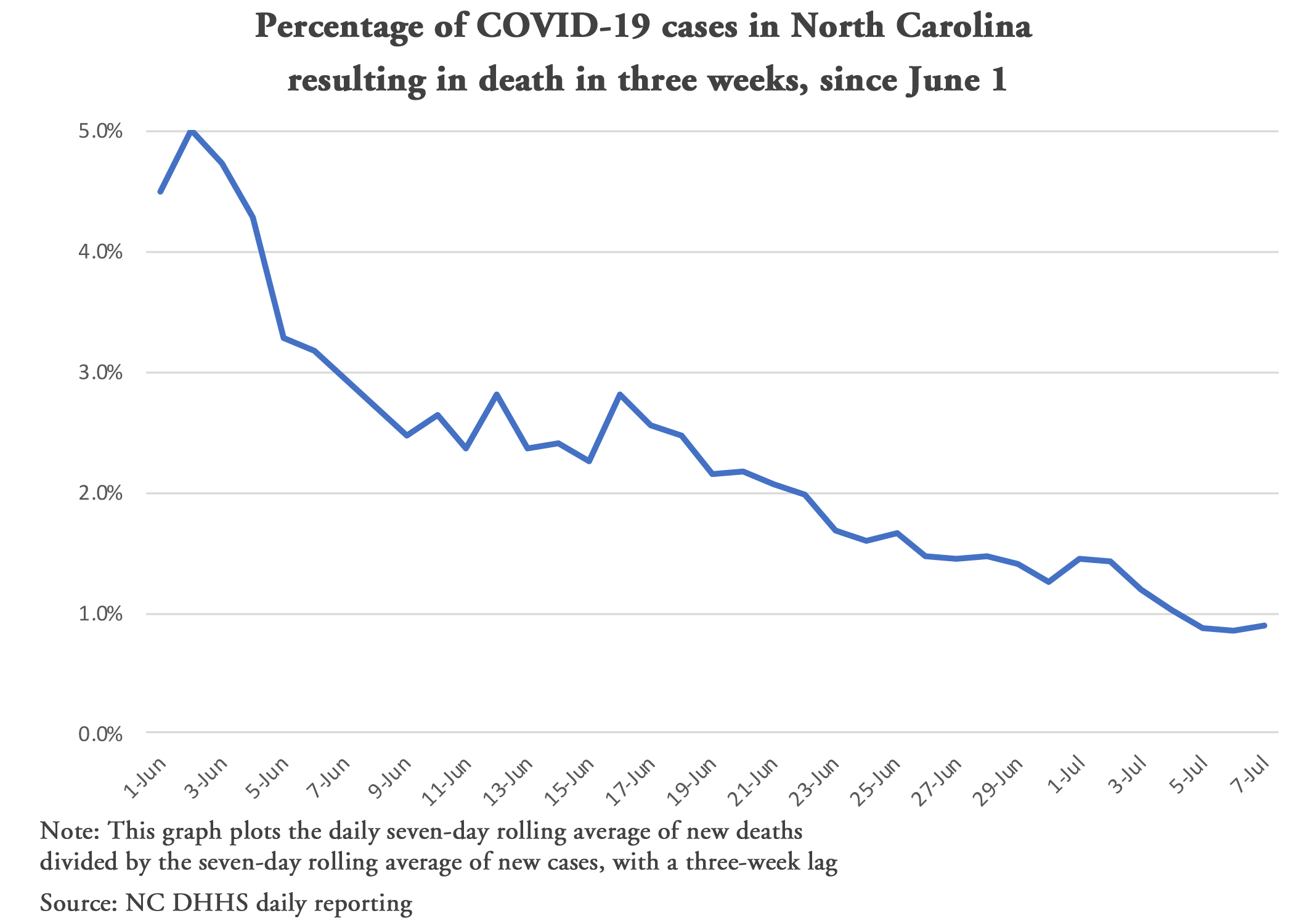
The choice of a lag of three weeks is somewhat arbitrary, but it is a reasonable assumption for mortality from a COVID-19 diagnosis and some would be captured in the 7-day rolling averages.
If there’s a trend, it should be visible and help us determine what we’re seeing with reported new cases. Is it more a dangerous rise in the virus itself, as media and the Cooper administration are promoting? Or is it more a result of more extensive testing finding the more asymptomatic or barely symptomatic (“not sick enough for medical care”) cases that weren’t included in the first few months’ worth of testing?