North Carolina is on track to reform its Medicaid program from one that pays physicians based on the number of services they deliver to patients to one in which commercial managed care companies will pay providers a defined amount of money per month to cover their patients’ medical needs.
The Department of Health and Human Services (DHHS) has already submitted a waiver to Washington last year in order for these changes to take effect. If all goes according to plan, key elements of Medicaid reform will be implemented starting in 2019.
But after hearing public input from special interests at a series of forums across the state, DHHS is set to submit another round of revisions to the original waiver. You can access the detailed proposal here. There are certainly some positive aspects, like telehealth initiatives and ensuring that health plans integrate behavioral and physical health care services for enrollees. But, one thing to be wary of is DHHS’s mindset to endorse Obamacare’s Medicaid expansion:
Enrollment Issues
- Medicaid was originally designed to provide coverage to low income children, adults, pregnant women, elderly, blind, and disabled. Expanding Medicaid will only further deteriorate access to care and puts current program beneficiaries at risk. A clear majority of new eligibles are working, do not have dependents to provide for, are not burdened with disabilities, and do not qualify for food stamps or other forms of public aid. In other words, those in support of expanding Medicaid would divert resources away from the traditional Medicaid population – not to mention that there are currently 17,000 North Carolinians on Medicaid waiting lists who suffer from severe physical and developmental disabilities.
Cost Issues
- According to the latest Centers for Medicare and Medicaid Services (CMS) report, Medicaid expansion enrollees cost 50 percent more than originally projected, adding an additional $19 billion to the already financially unstable program.
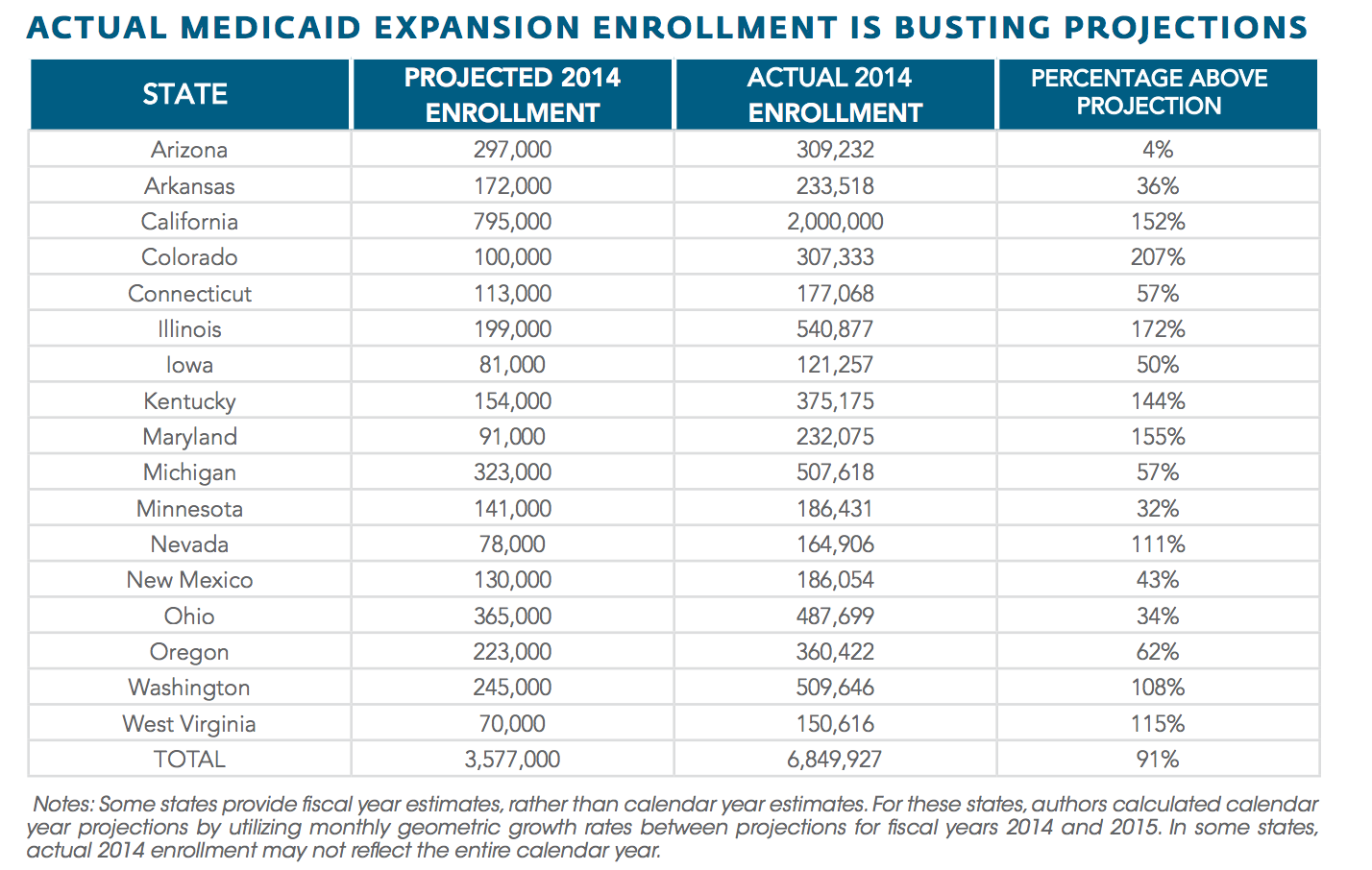
- In states that have expanded Medicaid eligibility, enrollments have far exceeded original projections, resulting in hundreds of millions of dollars in budget shortfalls. The Foundation for Government Accountability provides a state-by-state snapshot from fiscal year 2014: