North Carolina legislators are waiting for the feds to approve its 1115 waiver to reform Medicaid, the state-federal health insurance program that covers low-income parents, children, the elderly, blind, and disabled.
What’s the $14 billion program supposed to look like in the coming years?
Legislation to reform the program was signed into law at the close of the 2015 long session. One of its primary goals is to keep up with the trend in which payers are increasingly reimbursing doctors, hospitals, and health care providers based on value and less on volume (fee-for-service). For example, The Centers for Medicare and Medicaid Services (CMS) has reached its milestone of linking 30 percent of Medicare payments to quality or value-based outcomes. Plans to tie 60 percent of Medicare payments to quality metrics is set for 2018.
Another goal is to better manage care and further improve health outcomes for patients. This is why statewide commercial managed care organizations and provider-led plans are going to be held accountable to take on the risk for the patients they care for. Taking on risk is certainly no easy task, which is why reform isn’t going to happen over night. Passing legislation to change the administration of Medicaid has been a heavy lift over the last three years, and full reform won’t take effect until 2019 if all goes according to plan. See the timeline below taken from the 1115 waiver application that was shipped off to Washington on June 1:
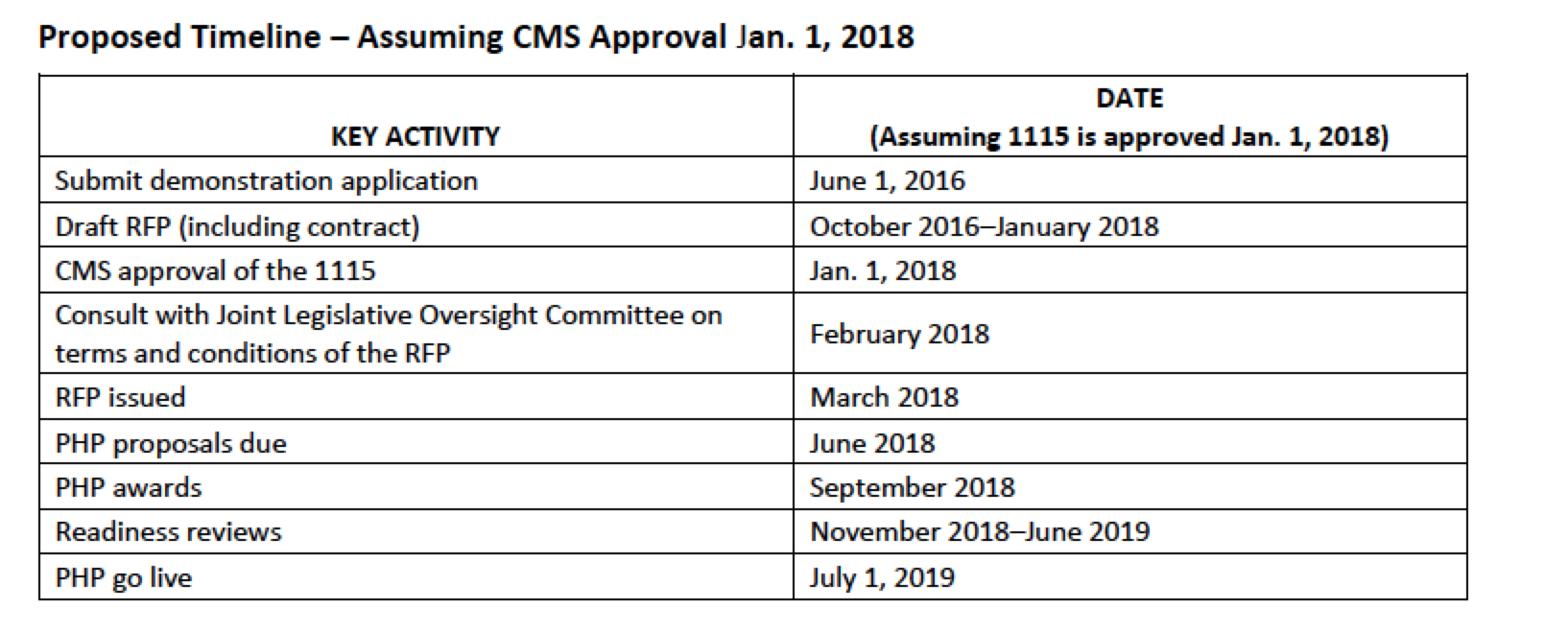
some highlights:
- The Request for Proposal (RFP) process is when Medicaid officials will determine which types of providers and what types of services will need to be covered in plans that will be formulated by hospital systems and commercial insurers. It’s important to note that North Carolina’s Medicaid waiver does not include an “any willing provider” clause – a key distinction from other states’ Medicaid managed care programs. In other words, health plans are not required to include any provider that agrees to the going rate for services set forth by the entities managing these plans. This is arguably a good thing, since reform merely doesn’t focus on cost containment. Those accepted into health plans will have to meet outlined quality standards as well.
- Overall, reform calls for 3 statewide managed care plans and up to 12 regional plans developed by provider-led organizations located in 6 different regions across the state.


